Table of Contents
- The Centers for Medicare & Medicaid Services (CMS) data system ...
- Medicaid coverage expands in W.Va. | News | fayettetribune.com
- 10 Things to Know About the Unwinding of the Medicaid Continuous ...
- Make Ends Meet: Medicaid coverage changes - YouTube
- CMS Requests Extended Special Enrollment Period for Individuals Losing ...
- Getting into Gear for 2014: Shifting New Medicaid Eligibility and ...
- Medicare Part D Disclosures due by March 1, 2017 for Calendar Year ...
- Five answers as CMS ends another year - EducationNC
- These states will see the biggest impact if Congress ends Medicaid ...
- State Medicaid Termination Timelines - YouTube


Background on Medicaid Funding



CMS Announcement


Implications for States
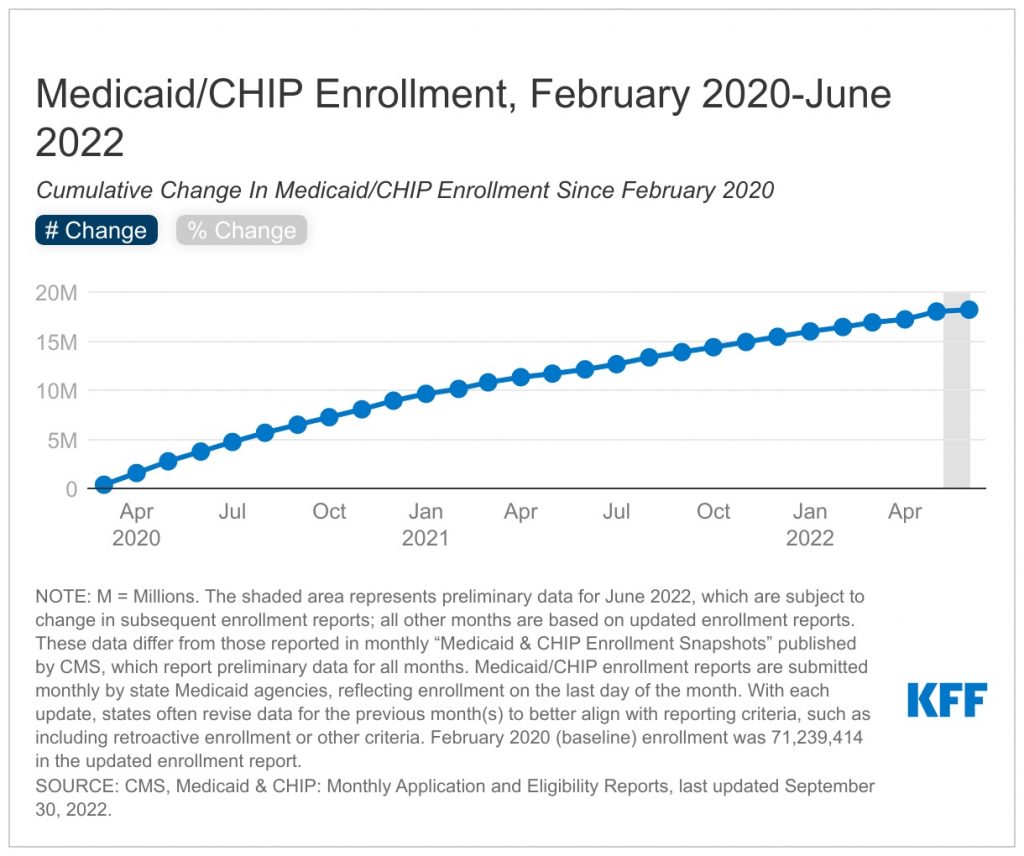
The CMS announcement is expected to have significant implications for state Medicaid programs. Without federal matching funds, states will be forced to absorb the full cost of their Medicaid programs, which could lead to: Reduced Medicaid enrollment: States may be forced to reduce Medicaid enrollment to manage costs, which could leave thousands of low-income individuals and families without access to healthcare coverage. Cuts to Medicaid benefits: States may be forced to cut Medicaid benefits, such as dental, vision, or prescription drug coverage, to manage costs. Increased state budget burdens: The loss of federal matching funds will place a significant burden on state budgets, which could lead to tax increases or cuts to other vital public programs.
Implications for Medicaid Beneficiaries
The CMS announcement will also have significant implications for Medicaid beneficiaries. Without access to federal matching funds, states may be forced to: Reduce provider reimbursement rates: States may reduce reimbursement rates for healthcare providers, which could lead to reduced access to care for Medicaid beneficiaries. Limit access to specialty care: States may limit access to specialty care, such as mental health or substance abuse treatment, to manage costs. Increase out-of-pocket costs: States may increase out-of-pocket costs, such as copays or coinsurance, for Medicaid beneficiaries to manage costs. The CMS announcement to end federal matching funds for states' Medicaid funding requests is a significant development that will have far-reaching implications for state Medicaid programs and Medicaid beneficiaries. As states struggle to manage the costs of their Medicaid programs, it is essential that policymakers prioritize the needs of low-income individuals and families who rely on Medicaid for healthcare coverage. We will continue to monitor the situation and provide updates as more information becomes available.Keyword: Medicaid, CMS, federal match, state funding, healthcare coverage